Like many millennials whose Sisyphean task is to assist their boomer parents with technology, I visited my mom in January to help facilitate a video call with a nurse practitioner. I found her pacing up and down the hallway.
“Hi, Janet!” I greeted her. “I’m your daughter Devon.”
“Oh!” she said, as if she knew she should recognize me, but did not. I asked her how she was doing. “I feel scared,” she replied.
“Why do you feel scared?” Her answer was a nonsensical jumble of words. She was able to articulate her feeling, but not the underlying reason. I venture she was scared because she didn’t know where or when she was. I’d be scared, too.
During the video call, I cringed as the nurse practitioner explained my mom would be reevaluated for hospice in the coming weeks. I tried not to say the word “hospice” in front of her, even though she’d been on it for six months. I glanced at her nervously, wondering if the word penetrated her consciousness. She stared out the window of her room, clenching the wooden slats of the blinds with both hands. When she’s nervous or upset about what’s going on around her, she tends to grip the nearest object. Her entire world has slipped away; she is desperate to hold onto something.
I’ve spent the last six years watching my mom deteriorate, and it’s been five years since we discovered why.
At 37, I am an early survivor of this specific hell. It’s quiet here. After her diagnosis at age 61, it took me more than a year to be able to speak the words aloud: “My mom has Alzheimer’s disease.” Even then, I could only whisper it between sobs.
Eventually I found a virtual support group for adult children of parents with early onset Alzheimer’s—the kind that strikes before the age of 65—and a handful of us whispered to each other over Zoom once a month. I began sharing my experiences on social media and more people my age came out of the woodwork to say they, too, are slowly and silently losing a parent.
“She’s in the end stage now and it’s the worst thing I’ve ever seen,” one woman in her thirties wrote to me about her mother. “I haven’t met anyone else with a similar experience.”
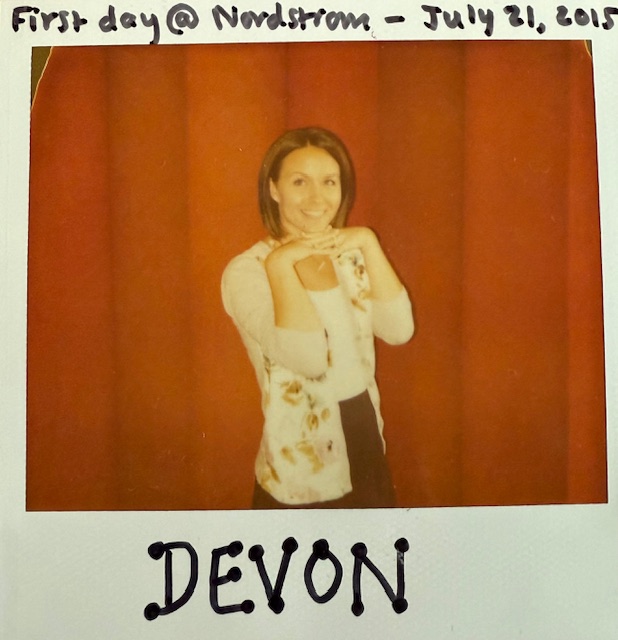
Alzheimer’s was never on my radar; there is no record of it running on either side of my family. My mom was a highly capable executive assistant who spent her free time quilting and tending to her vegetable garden. She looked forward to retirement and becoming a grandmother. I’ll always remember how she danced around my living room in 2015 when I shared the news of my pregnancy. I didn’t expect to rejoice over my daughter learning how to use the toilet, dress herself and read at the same time my mom lost those abilities.
We certainly never discussed how things might play out if she were to develop dementia. It’s a conversation I didn’t think to have—and might have been afraid to have, as if saying “Alzheimer’s” aloud could conjure it into reality. Still it crept up on my mom, stealthy and vicious, and stole her from me piece by piece.
My friends—most of whom have healthy parents who host holiday dinners and babysit their kids on weekends—sympathize, but can’t relate. It’s my lonely reality right now. But like the Stark family in “Game of Thrones,” I issue an ominous warning to my fellow millennials: Dementia is coming.
I’ve seen it with my own eyes; I’ve heard it in the whispers. And the statistics are grim. The Alzheimer’s Association estimates 6.9 million Americans age 65 and older are living with Alzheimer’s dementia in 2024. It projects this number will balloon to 12.7 million by 2050.
I worry about the onslaught of devastation that’s coming for boomers and their millennial children. Our parents are the ones who swept us back into the nest during the Great Recession, kept us on their health insurance plans until we turned 26, and opened up guest rooms and basements to us temporarily—and not so temporarily—during the pandemic. Many of us are still paying off decades-old student loans. We’re unprepared to not only lose our parents’ support, but to muster all our energy and resources to support them.
How many boomers have long-term care insurance or the savings to fund long-term care? How many of their children realize they will be the ones to provide or pay for this care? Are there enough neurologists to diagnose millions of new Alzheimer’s cases? Enough home health-care workers to support family caregivers? Enough memory-care facilities to house patients? Enough therapists to help families survive the excruciating experience of losing a loved one over many years?
To echo my mom, I feel scared.
I’m not equipped to fix our health care system’s current and future failures around caring for Americans living with dementia and supporting their families, but I do have some advice on a personal level for families who may face this fate. It all starts with a conversation.
My family was completely unprepared for all the challenges of Alzheimer’s disease. Nothing will ease the heartbreak of an Alzheimer’s diagnosis, but making key decisions ahead of or shortly after a diagnosis can ease some heartache down the road for loved ones.
When my mom was diagnosed in November 2019, I thought we had plenty of time before we needed to discuss the details of her inevitable decline and confirm her wishes. But the initially slow progression of her disease accelerated into a freefall during the first year of the pandemic, and we were left scrambling for solutions from a place of panic. Once the window has closed for someone with dementia to make informed decisions about their future, loved ones are left to make their best guesses.
A survey by the Kaiser Family Foundation found that fewer than half of adults have seriously discussed long-term care plans with a loved one—including who will help take care of them and how they will pay for health care and other support they’ll need if they become seriously ill. And nearly 7 in 10 boomers will need long-term care in their remaining years according to the U.S. Department of Health and Human Services. Families should have open conversations now about the future, whether or not there is a history of dementia in the family.
Get real about finances.
Discuss the resources you’ll have available to pay for care. The cost of caring for someone with a progressive neurodegenerative disease is staggering, and the truth about who pays for it can be summed up by one of fellow millennial Taylor Swift’s songs: “You’re On Your Own, Kid.”
Medicare only pays for long-term care if you require skilled services or rehabilitative care in a nursing home for a maximum of 100 days; that hardly scratches the surface of the amount of care needed for someone with dementia who typically declines over several years. Medicaid may cover some long-term care costs, but only for those with very limited financial means. Long-term care insurance can help, but be sure to review policy details and coverage limitations. Veterans may be eligible for benefits through the Department of Veterans Affairs. My friend Lauren, who cared for her grandmother with Alzheimer’s and previously worked for the Alzheimer’s Association, advises to “check out your state’s aging department or your local Area Agency on Aging (AAA). Each state is different and some have bridge programs for people with Alzheimer’s or other diseases that can be a stipend to pay for assisted living or memory care until someone qualifies for Medicaid. In some cases there are home-care grants, and others will pay for facility-based care.”
But many families—like mine—rely on personal savings and home equity to pay for care. My mom’s husband Don was initially determined to care for her at home, but in the darkest days of the pandemic, the emotional and physical toll it took on him was clear and cruel. “We can’t save her,” I told him, “but maybe we can still save you.” We moved her into a memory care facility near Seattle, which over the past four years has drained hundreds of thousands of dollars from the retirement savings they worked so hard to build. The monthly cost has risen to more than $13,000. We are counting down the months until we’ll need to sell their home.
It’s a stark reality many Americans face, as detailed in the New York Times series “Dying Broke,” and few people realize it until it’s too late to prepare. Try calculating the median costs of care in your area—including in-home care, adult day care and full-time care in a facility—and consult with a financial advisor to get personalized guidance based on your circumstances.
Talk through medical options.
Alzheimer’s disease is invariably fatal, but there are medications and experimental treatments that may help manage symptoms or slow the progression. Discuss whether or not you’d want to take medications or participate in a clinical trial.
My mom began taking two medications immediately after her diagnosis. I realized in the spring of 2023 that her quality of life had declined to the point where it no longer made sense to attempt to slow the progression of the disease and, after many discussions with family members and her doctor, we tapered her off the medications. Even though I felt this was the right decision—the one she likely would have made if she could—making it was agonizing. My mom had a standard advance health care directive, but it did not account for the nuances of dementia care. How I longed for a clear record of her wishes.
Consider filling out the dementia-specific advance directive created by Dr. Barak Gaster, an internist at the University of Washington Medical Center. Discuss it with loved ones, and share copies of it with them and with health care providers. The Conversation Project also provides a guide to determining what matters most to someone living with dementia so they can have a say in their health care.
I agonized for months over whether my mom needed to endure her decline at all. Would she have wanted to end her own life instead? Should I have helped her explore options while she was still capable of carrying out a plan? The answer, it turned out, was no. Once I felt brave enough to broach the topic, Don assured me her Catholic upbringing made the idea impossible. Having no religious roots myself—and having witnessed her suffering up close—I can’t say I’d have the same answer if I find myself in her shoes someday.
It’s worth discussing where you stand on the idea and considering the options, which do not include medical aid in dying in the U.S. Even in the states where it’s legal, people with dementia are excluded from utilizing it due to two of the requirements: once they have less than six months to live, they are no longer able to make and communicate an informed decision to health care providers.
However, it filled me with great peace to read Amy Bloom’s beautiful memoir “In Love,” which chronicles her husband’s decision following an Alzheimer’s diagnosis to end his life with the help of Dignitas, a Swiss nonprofit organization. I also learned about voluntarily stopping eating and drinking, and read with great interest “The Last Day of Her Life,” a New York Times Magazine feature about how Cornell psychology professor Sandy Bem orchestrated an early exit on her own terms.
Complete and share important paperwork.
In addition to having a standard will and estate plan in place, it’s crucial to record all financial and health care wishes in the following legal and medical documents. Consider working with an attorney who specializes in estate planning or elder law to cover all your bases.
Discuss the details of these documents with the people who will be responsible for carrying out your wishes, and share copies with them and with health care providers. Don’t skip the sharing part; no one can follow your directions if they don’t know they exist.
Durable financial power of attorney: Designate an agent (and at least one backup) to make decisions regarding your money, property and belongings if you lose the capacity to do so. Following a dementia diagnosis or other mentally incapacitating health event, the agent should contact every entity involved with your finances—including Social Security, Medicare, the IRS, insurance companies, banks and utilities—to complete any paperwork required for them to recognize the agent as the sole executor of your accounts. For example, the Treasury Department doesn’t recognize power of attorney for handling federal payments like Social Security; one must separately apply to serve as a person’s representative payee.
Don described the entire process of taking control of my mom’s finances as a total nightmare. He was met with red tape at every turn, and had to physically bring my mom to several offices along with documentation from her neurologists regarding her diagnosis and mental incapacity. It was incredibly stressful for both of them. “If she had been any more incapacitated”—at the time, she was still able to hold a normal conversation and sign documents—“I don’t know how I would have possibly done it,” he said.
Advance health care directive or living will: Specify what actions should be taken for your health if you lose the capacity to make decisions. Make clear your wishes regarding artificial life support and more.
Durable health care power of attorney: Designate an agent (and at least one backup) to make health care decisions for you if you lose the capacity to do so. Discuss your wishes with these agents and make sure they are comfortable carrying them out.
Do not resuscitate (DNR) order: This medical document instructs health care providers not to perform CPR or other life-support procedures if your heart or breathing stops. Discuss your wishes with your physician, who will fill out the form.
Portable medical orders (POLST): This medical document is more specific than a DNR or advance health care directive and is for people who already have a severe illness, like dementia. The form and its exact name vary by state, but it communicates your wishes as medical orders, including whether or not you want CPR, to be transported to a hospital and to receive medically assisted nutrition. Discuss your wishes with your physician, who will fill out the form.
Millennials: Plan for your future now.
The longer we live, the more our risk of dementia increases. The time is now for millennials to prepare for our own potential long-term care needs.
If you’ve held off on contributing to a 401(k), IRA or other retirement savings plan: start today. If you already contribute and are able to increase the amount: start today. If you’ve never even heard of long-term care insurance or looked into applying for it: start today.
I felt hopeful in 2019 when Washington state established the WA Cares Fund, a first-in-the-nation mandatory long-term care insurance program, but almost laughed when I saw the maximum benefit is $36,500 (adjusted up to inflation). It’s a drop in the bucket for someone with dementia. But still, it’s better than nothing, and far more than what many Americans have planned for their long-term care.
If you have any assets, a spouse or children, it’s essential to have a will and estate plan in place, and to create a record of your financial and health care wishes before you’re no longer able to do so. You can always change them later.
Let’s break the silence.
Alzheimer’s is the most-feared disease of older Americans, and the only one of the top 10 causes of death in the U.S. with no known cure. The stigma around Alzheimer’s causes people to live with it in silence and shame, and their families to grieve in silence and shame as well. Some call it a family disease because of the devastating impact it has on loved ones’ mental and physical health.
I’m done whispering. Now I’m yelling: Dementia is coming, but we don’t have to suffer through it alone.
I’m encouraged by my generation’s propensity to share our struggles, thanks to social media, and to embrace therapy and support groups. I believe many of us will cope with losing our parents by shedding light on our darkest experiences. It makes a world of difference to connect with others enduring the same heartbreak. The Alzheimer’s Association has a 24/7 helpline (800.272.3900) and offers support groups and a free online community for people living with dementia and their loved ones.
The greatest tragedies are made even worse by our failure to learn from them. And the lessons we learn are made even more valuable when we share them.
I still can’t save my mom, nor the millions of boomers who will be diagnosed with Alzheimer’s in the coming decades. Maybe I can, in some small way, help save the people who love them.